Can Acidity Feel Like a Heart Attack? How to Tell the Difference
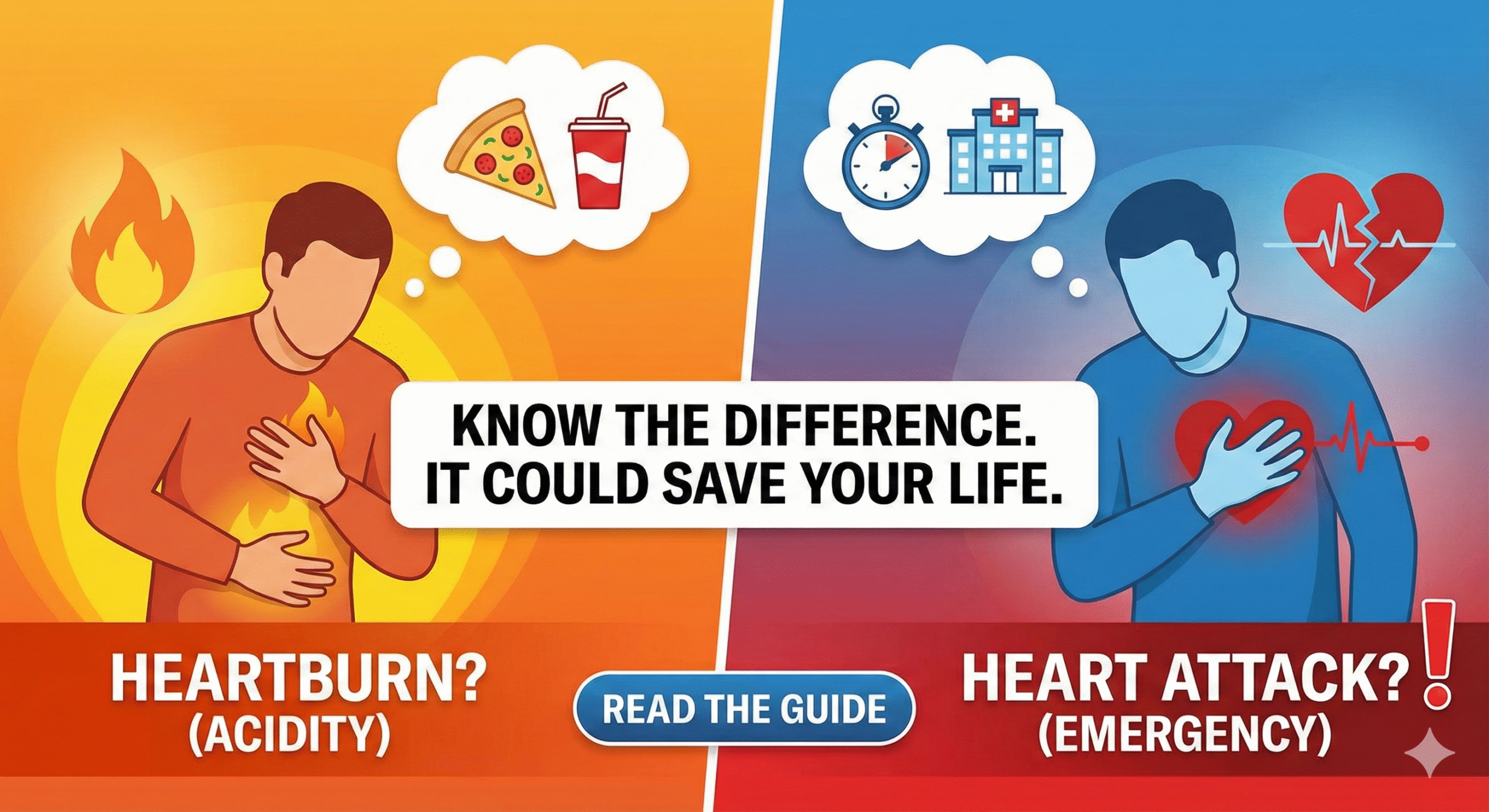
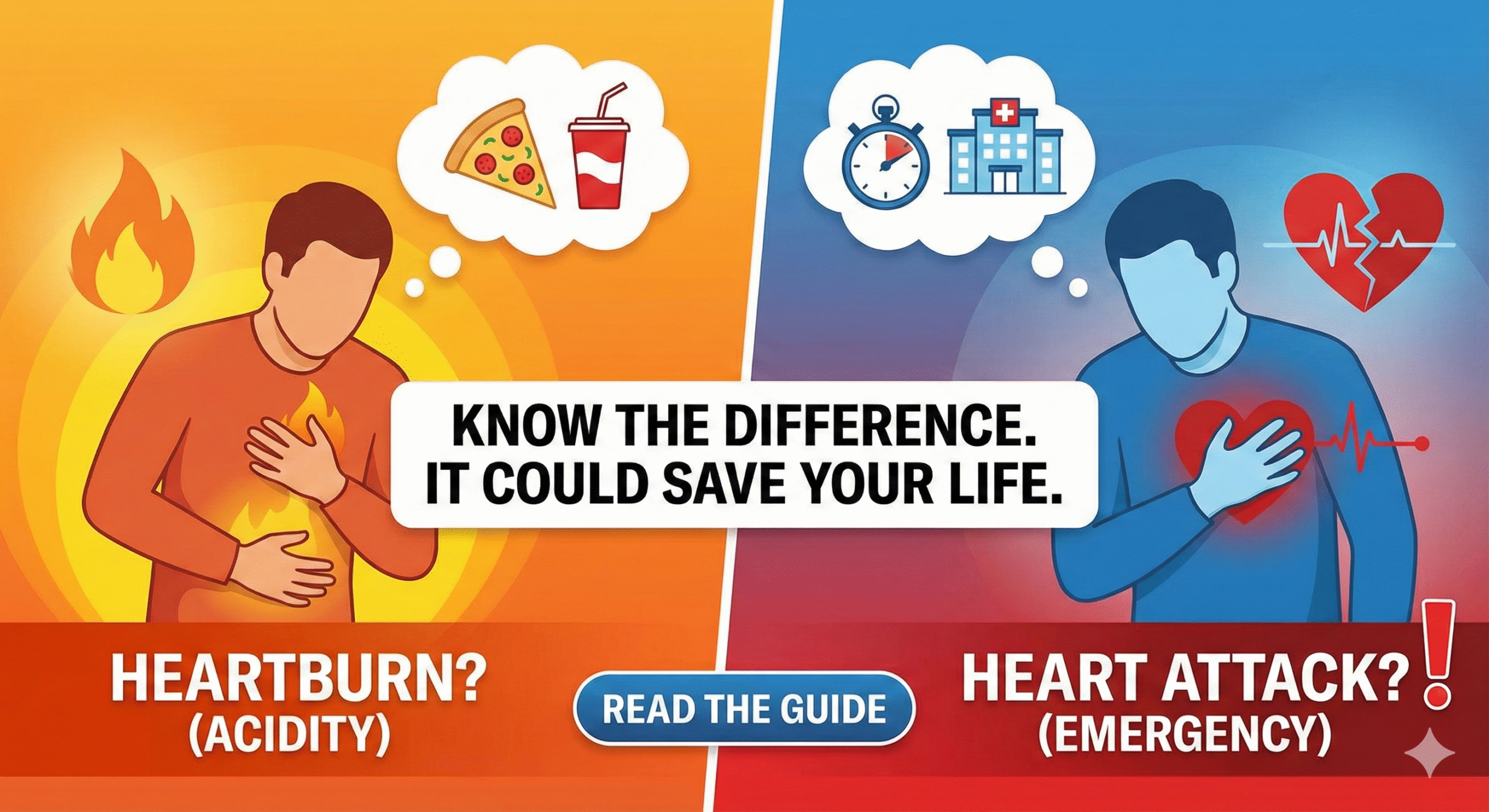
Can Acidity Feel Like a Heart Attack? How to Tell the Difference
Acidity feel like a heart attack – this is not just a common worry, but a real medical puzzle that sends thousands of people to emergency rooms every year. If you’ve ever felt a crushing pain in your chest after a meal, you know how scary it can be. Is it your heart or just your stomach? Understanding the difference could save your life.
Acidity, also called acid reflux or heartburn, happens when stomach acid flows back into the food pipe (esophagus). This creates a burning sensation in chest that can feel very similar to heart-related pain. The esophagus runs right behind your heart, which is why the pain locations overlap.
When you eat, a ring of muscle at the bottom of your esophagus (called the lower esophageal sphincter) relaxes to let food pass into your stomach. Sometimes, this muscle doesn’t close properly, allowing acid to splash back up. This is the main cause of gastroesophageal reflux disease symptoms.
For people with heart disease or diabetes, this confusion becomes even more dangerous. Your body might be giving you warning signs, but you could easily dismiss them as simple indigestion.
A heart attack occurs when blood flow to a part of your heart muscle gets blocked. This causes damage to the heart tissue and creates chest pain that doctors call angina. The key difference between angina vs acid reflux lies in several important factors.
Heart attack pain typically:
According to a Harvard Medical Study, about 50% of people experiencing a heart attack don’t realize what’s happening initially. For diabetic patients, this number is even higher because diabetes can damage nerves, reducing pain sensation.
Understanding the difference between indigestion and heart problems can literally save your life. Here’s what you need to know:
Acidity:
Heart Attack:
Acidity:
Heart Attack:
Acidity symptoms include:
Heart attack warnings include:
Recent clinical trials suggest that misdiagnosis between acid reflux chest pain vs heart attack is alarmingly common. A study published in the American Journal of Medicine found that:
These numbers show why you should never assume chest pain is “just acidity” without proper medical evaluation, especially if you have risk factors like diabetes, high blood pressure, or heart disease.
Never wait if you experience any of these symptoms. Call emergency services immediately:
For diabetic and heart patients, even mild symptoms deserve attention. Your body might not send strong pain signals due to nerve damage from diabetes.
When you visit a doctor with chest pain, they will perform several tests to determine if you’re experiencing acidity feel like a heart attack or an actual cardiac event:
| Treatment Type | For Acidity/GERD | For Heart Disease | Timeline | Effectiveness |
|---|---|---|---|---|
| Lifestyle Changes | Diet modification, weight loss, avoiding triggers | Exercise, stress management, healthy diet | 2-4 weeks | 60-70% improvement |
| Medications | Antacids, H2 blockers, PPIs (Proton pump inhibitors) | Beta-blockers, ACE inhibitors, statins, aspirin | 1-2 weeks | 80-90% symptom control |
| Minimally Invasive | Endoscopic procedures, TIF surgery | Angioplasty, stenting | Immediate | 85-95% success |
| EECP Therapy | Not applicable | Enhanced External Counterpulsation for angina | 7 weeks (35 sessions) | 75-85% symptom relief |
| Surgery | Fundoplication (for severe GERD) | Bypass surgery, valve repair | Recovery: 4-6 weeks | 90-95% long-term success |
Many patients prefer starting with natural remedies before moving to stronger medications. Here are evidence-based options:
Important Note: While natural remedies can help with mild acidity, always consult your doctor if symptoms persist or worsen. Never use natural treatments as a substitute for emergency care if you suspect a heart attack.
Enhanced External Counterpulsation (EECP) therapy is a revolutionary treatment for patients with chronic angina and heart disease. This non-invasive procedure uses external pressure to improve blood flow to your heart.
During treatment, inflatable cuffs are wrapped around your calves, thighs, and buttocks. These cuffs inflate and deflate in sync with your heartbeat, pushing oxygen-rich blood back to your heart and creating new pathways around blocked arteries.
According to recent clinical trials, 75-80% of patients experience significant improvement after completing the full EECP therapy course. The treatment typically involves 35 one-hour sessions over 7 weeks.
Certain conditions make you more likely to experience both serious acid reflux and heart disease:
If you have multiple risk factors from both lists, you need to be extra careful about evaluating chest pain symptoms.
If you have diabetes, distinguishing between acidity and heart attack becomes more challenging because:
A study from the American Diabetes Association found that diabetic patients are 2-4 times more likely to have heart disease and often experience atypical symptoms. This means you should have a lower threshold for seeking medical care when experiencing chest discomfort.
If you frequently experience chest pain, ask your doctor about these tests:
Having baseline results helps doctors quickly identify changes when acute symptoms occur.
Both conditions require ongoing management:
Never stop medications without consulting your doctor, even if symptoms improve.
At NexIn Health, we understand the complexity of managing heart disease, diabetes, and related conditions. Our team specializes in non-invasive integrated techniques that combine the best of modern medicine with holistic approaches.
With over 14 years of experience and 30,000+ patients consulted, we offer comprehensive heart and spine treatment through advanced therapies including EECP, lifestyle modification programs, and personalized care plans. Our experts help you distinguish between cardiac and non-cardiac chest pain while providing cutting-edge treatment options.
Don’t let confusion about chest pain put your life at risk. Get expert evaluation and treatment today.
Contact NexIn Health:
Que: Can acidity feel like a heart attack even if I have no heart disease history?
Ans: Yes, severe acid reflux can cause chest pain that feels identical to a heart attack, even in people with healthy hearts. The esophagus is located right behind the heart, so inflammation or acid irritation can cause intense chest discomfort. However, never assume chest pain is “just acidity” without medical evaluation, especially if it’s your first episode or feels different from usual heartburn.
Que: How quickly should I seek help if I’m unsure whether it’s acidity or a heart attack?
Ans: If chest pain lasts more than 5 minutes, is severe, or comes with shortness of breath, sweating, or pain spreading to your arm or jaw, call emergency services immediately. For heart patients and diabetics, seek help even sooner. It’s always better to get checked and find it’s acidity than to wait and suffer a heart attack.
Que: Can taking antacids help me figure out if it’s acidity or heart attack?
Ans: While antacids may relieve acid reflux within 5-10 minutes, relying on this test is dangerous. Heart attack pain won’t respond to antacids, but some cases of both conditions can occur together. Never use the “antacid test” as a diagnostic tool. If you’re experiencing chest pain and are unsure, seek immediate medical attention.
Que: Why do diabetic patients have more difficulty telling the difference?
Ans: Diabetes can damage nerves (diabetic neuropathy), reducing your ability to feel pain. This means a heart attack might present with milder symptoms or unusual signs like nausea, fatigue, or shortness of breath rather than severe chest pain. Diabetics should maintain extra vigilance and have a lower threshold for seeking medical care with any chest discomfort.
Que: Can GERD increase my risk of having a heart attack?
Ans: GERD itself doesn’t directly cause heart attacks, but both conditions share common risk factors like obesity, poor diet, and sedentary lifestyle. Some studies suggest chronic inflammation from GERD might contribute to cardiovascular risk. Additionally, having GERD can make it harder to recognize heart attack symptoms, potentially delaying life-saving treatment.
Que: What lifestyle changes work for both preventing heart disease and reducing acidity?
Ans: Maintaining healthy weight, eating smaller meals, reducing fatty and processed foods, avoiding smoking and excessive alcohol, managing stress, and regular exercise all benefit both conditions. For heart patients with diabetes, controlling blood sugar levels is especially important as it reduces risk for both cardiac events and worsening GERD.
Que: Is EECP therapy safe for patients who also have severe acid reflux?
Ans: Yes, EECP therapy is generally safe for patients with GERD. The treatment involves lying down with pressure cuffs on your legs, which shouldn’t aggravate acid reflux. However, inform your doctor about your GERD symptoms. They may recommend avoiding eating for 2-3 hours before treatment sessions and possibly adjusting your reflux medications during the therapy course.
Que: Can natural remedies completely replace medications for acid reflux in heart patients?
Ans: While natural remedies like ginger, fennel, and aloe vera can help manage mild symptoms, heart patients should never stop prescribed medications without consulting their doctor. Some natural supplements can interact with heart medications. Always discuss natural remedies with your healthcare provider before adding them to your treatment plan.
Que: How often should heart patients with frequent acidity get cardiac evaluations?
Ans: If you have heart disease and experience frequent chest discomfort from acidity, discuss with your cardiologist about appropriate screening intervals. Generally, annual ECG and stress tests are recommended, but if symptoms change or become more frequent, earlier evaluation is necessary. Keep a symptom diary to help your doctor distinguish between cardiac and non-cardiac episodes.
Que: What emergency information should I keep handy if I have both heart disease and GERD?
Ans: Keep a list of all medications, known allergies, your doctors’ contact information, recent test results, and a brief medical history. Wear a medical alert bracelet if you have diabetes or heart disease. Share your action plan with family members so they know when to call emergency services. Keep emergency numbers programmed in your phone and easily accessible at home.
Final Thoughts
Understanding whether acidity feel like a heart attack or if you’re experiencing a true cardiac emergency can be life-saving knowledge. While chest pain from acid reflux is common and usually not dangerous, you should never ignore chest discomfort, especially if you have diabetes, heart disease, or other risk factors.
The key is knowing your body, recognizing warning signs, and seeking help when in doubt. With proper medical care, lifestyle modifications, and treatments like EECP therapy, you can manage both conditions effectively and live a healthy, active life.
Remember: when it comes to chest pain, it’s always better to be safe than sorry. Trust your instincts and seek medical attention if something feels wrong.