What is Coronary Artery Disease
Did you know that out of all the diseases we know today, the disease that causes the most fatalities on earth isn’t considered to be an ‘illness’ but rather a ‘condition’ that causes trouble to millions without the common knowledge of many?💔 I am talking of Coronary Artery Disease, or CAD, which is one of the worst diseases that one can have but is still neglected by many including professionals. It is also equally important to mention that CAD does not care about your age or where you are from, for it affects everyone across the globe who tends to be a human.
Consider this: your heart is a solid engine and the coronary arteries are its fuel lines, and as time passes those fuel lines begin to shrink. This ends up restricting blood flow to the heart even with these basic side effects and at times, leaves patients in a very critical situation. But this may be the most shocking aspect of it all: until it is too late in life, you may not even be aware that you have it. By the end of this article, you will get a far better understanding of CAD from its fundamental concepts to how you can reverse it by using natural means. Let’s see if we can find out how to mitigate the risks associated with this routine issue but can be life threatening. The ultimate goal would be to keep our hearts healthy for a long period of time.
Coronary Artery Disease (CAD) can be defined as a heart condition caused by reduced blood flow in the arteries, known as the coronary arteries. Arteries are usually 2-4 mm wide and their function is to provide blood to various parts of the body, in this case, the heart.
| Artery | Area Supplied |
|---|---|
| Left anterior descending | Front and side of left ventricle |
| Left circumflex | Side and back of left ventricle |
| Right coronary | Right ventricle and back of left ventricle |
CAD develops when plaque, consisting of cholesterol, fat, and other substances, accumulates in the arterial walls. This process, known as atherosclerosis, leads to reduced blood flow to the heart.
High blood pressure
High cholesterol levels
Smoking
Diabetes
Obesity
Sedentary lifestyle
Family history of heart disease
Age (risk increases with age)
Coronary Artery Disease remains a leading cause of death worldwide, with varying prevalence across different demographics.
| Demographic | Prevalence Trend |
|---|---|
| Age | Increases with age, more common after 65 |
| Gender | Higher in men, risk equalizes post-menopause for women |
| Ethnicity | Higher rates in South Asians and African Americans |
Recent trends show a decline in CAD-related mortality in developed countries due to improved prevention and treatment strategies. However, the prevalence is rising in developing nations due to lifestyle changes and increased life expectancy.
Now that we’ve established a foundation for understanding Coronary Artery Disease, let’s explore the symptoms and warning signs that individuals should be aware of to detect this condition early.
The classic symptoms of Coronary Artery Disease (CAD) are often described as:
Chest pain or discomfort (angina)
Shortness of breath
Heart palpitations
Fatigue or weakness
Nausea
| Symptom | Description |
|---|---|
| Chest pain | Pressure, squeezing, or burning sensation in the chest |
| Shortness of breath | Difficulty breathing, especially during physical activity |
| Heart palpitations | Irregular or rapid heartbeat |
| Fatigue | Unusual tiredness, even with minimal exertion |
| Nausea | Feeling sick to the stomach, often accompanied by other symptoms |
Not everyone experiences the classic symptoms of CAD. Atypical presentations may include:
Pain in the jaw, neck, throat, or back
Indigestion or heartburn
Lightheadedness or dizziness
Cold sweats
Unexplained anxiety
It’s crucial to recognize when symptoms require immediate medical attention:
Chest pain lasting more than a few minutes
Severe shortness of breath
Fainting or loss of consciousness
Sudden weakness or numbness in limbs
Women may experience CAD symptoms differently than men:
| Men | Women |
|---|---|
| More likely to have classic chest pain | May have subtler, less recognizable symptoms |
| Often report pain in left arm | May experience pain in both arms, back, or jaw |
| Typically sudden and intense symptoms | Symptoms may develop gradually |
| Less likely to experience nausea | More likely to experience nausea and vomiting |
Understanding these differences is crucial for early detection and treatment of CAD in both genders. Now that we’ve covered the symptoms and warning signs, let’s explore the various methods used to diagnose and screen for Coronary Artery Disease.
The first step in diagnosing coronary artery disease (CAD) involves a comprehensive physical examination and medical history review. Your doctor will:
Check your blood pressure, heart rate, and overall physical condition
Listen to your heart for abnormal sounds or murmurs
Assess risk factors such as family history, smoking, and diabetes
Non-invasive tests are crucial for detecting CAD without entering the body. Common tests include:
Electrocardiogram (ECG): Records electrical activity of the heart
Stress tests: Monitors heart function during exercise
Imaging tests: Provide detailed views of the heart and arteries
| Test Type | Purpose | Procedure |
|---|---|---|
| ECG | Detect irregular heartbeats | Electrodes placed on chest |
| Stress Test | Evaluate heart function under exertion | Walking on treadmill or cycling |
| Echocardiogram | Visualize heart structure and function | Ultrasound imaging |
When non-invasive tests are inconclusive, invasive procedures may be necessary:
Coronary angiography: Gold standard for diagnosing CAD
Involves inserting a catheter into arteries to inject contrast dye
Provides detailed images of coronary arteries and blockages
Several blood tests can help assess the risk and progression of CAD:
High-sensitivity C-reactive protein (hsCRP): Measures inflammation
Fasting insulin: Evaluates insulin resistance
HOMA (Homeostatic Model Assessment): Calculates insulin sensitivity
D-dimer: Indicates potential blood clots
Lipid profile: Measures cholesterol and triglyceride levels
These tests provide valuable insights into cardiovascular health and help guide treatment decisions. Regular monitoring of these markers can aid in tracking the progression of CAD and the effectiveness of interventions.
Coronary artery blockages tend to form in specific areas due to a combination of factors. These areas, known as atherosclerosis-prone regions, are often found at vessel branch points or areas of turbulent blood flow. Here’s why:
Hemodynamic stress: Areas with disturbed blood flow experience more mechanical stress on the arterial walls.
Endothelial dysfunction: These stressed areas are more prone to endothelial damage, leading to inflammation.
Lipid accumulation: Damaged areas trap more lipids, initiating plaque formation.
| Factor | Impact on Blockage Formation |
|---|---|
| Blood flow | Turbulent areas more prone |
| Vessel shape | Branching points at higher risk |
| Inflammation | Increases likelihood of plaque |
| Lipid levels | Higher levels accelerate buildup |
Blockage growth is a gradual process involving several stages:
Endothelial damage
Lipid accumulation
Inflammatory response
Smooth muscle cell proliferation
Fibrous cap formation
Plaque expansion and remodeling
This process, known as atherosclerosis, can take years or even decades to develop significant blockages.
Contrary to popular belief, it’s not always the largest blockages that pose the greatest risk for heart attacks. The most dangerous plaques are often:
Vulnerable plaques: These have thin fibrous caps and large lipid cores.
Inflamed plaques: High inflammatory activity increases rupture risk.
Positively remodeled plaques: These grow outward and may not cause significant stenosis.
Smaller blockages can be more dangerous because:
They’re often overlooked in screenings
They’re more likely to rupture due to thinner fibrous caps
They may not cause symptoms, leading to delayed treatment
They can grow rapidly and unpredictably
Large blockages, while significant, often develop collateral circulation and may be more stable.
A heart attack occurs when a blockage ruptures, leading to:
Plaque contents exposure to blood
Rapid blood clot formation
Complete vessel occlusion
Myocardial ischemia and necrosis
The rupture often happens due to physical or emotional stress, triggering a cascade of events that can result in a life-threatening heart attack. Understanding these processes is crucial for effective prevention and treatment of coronary artery disease.
Animals, particularly wild animals, have evolved over millions of years to develop natural defenses against heart disease. Their lifestyle and diet play crucial roles in protecting them from coronary artery disease. Here’s a comparison of human and animal cardiovascular health:
| Factor | Humans | Wild Animals |
|---|---|---|
| Diet | Processed, high-fat foods | Natural, nutrient-rich diet |
| Physical Activity | Often sedentary | Constant movement |
| Stress Levels | High chronic stress | Acute stress only |
| Lifespan | Longer, artificial environment | Shorter, natural environment |
Natural diet: Wild animals consume foods rich in antioxidants and omega-3 fatty acids
Regular physical activity: Constant movement promotes cardiovascular health
Stress management: Animals experience only acute stress, not chronic stress
Genetic factors: Natural selection favors cardiovascular health in the wild
While animals in captivity may develop heart problems similar to humans, their wild counterparts rarely suffer from coronary artery disease. This stark difference highlights the importance of lifestyle factors in preventing heart attacks. Understanding these natural protective mechanisms can provide valuable insights into preventing and managing coronary artery disease in humans.
Now that we’ve explored why animals don’t typically suffer from heart attacks, let’s examine how we can apply these lessons to reverse blockages naturally in humans.
One of the most effective ways to reverse coronary artery blockages naturally is through significant dietary modifications. A heart-healthy diet should focus on:
Whole, plant-based foods
Lean proteins
Healthy fats
Low-sodium options
Here’s a comparison of foods to embrace and avoid:
| Embrace | Avoid |
|---|---|
| Fruits and vegetables | Processed meats |
| Whole grains | Refined carbohydrates |
| Legumes | Sugary beverages |
| Nuts and seeds | Trans fats |
| Fatty fish | Excessive salt |
Physical activity plays a crucial role in reversing heart blockages. Aim for at least 150 minutes of moderate-intensity exercise per week. Consider:
Brisk walking
Swimming
Cycling
Yoga or tai chi
Chronic stress can contribute to heart disease. Implement stress-reduction techniques such as:
Meditation
Deep breathing exercises
Progressive muscle relaxation
Mindfulness practices
Additional lifestyle changes can significantly impact heart health:
Quit smoking
Limit alcohol consumption
Maintain a healthy weight
Get adequate sleep (7-9 hours nightly)
By incorporating these natural methods, you can potentially reverse coronary artery blockages and improve overall heart health. However, it’s essential to work closely with your healthcare provider to monitor progress and ensure these approaches complement any prescribed medical treatments.
Lifestyle modifications play a crucial role in managing coronary artery disease (CAD). These changes can significantly improve heart health and reduce the risk of complications. Here are some key lifestyle modifications:
Regular exercise (at least 30 minutes, 5 days a week)
Heart-healthy diet (low in saturated fats, high in fruits and vegetables)
Smoking cessation
Stress management techniques
Weight management
Various medications can help manage CAD symptoms and reduce the risk of heart attacks. Common medications include:
| Medication Type | Benefits |
|---|---|
| Statins | Lower cholesterol levels |
| Beta-blockers | Reduce heart rate and blood pressure |
| ACE inhibitors | Improve blood flow and lower blood pressure |
| Antiplatelet drugs | Prevent blood clots |
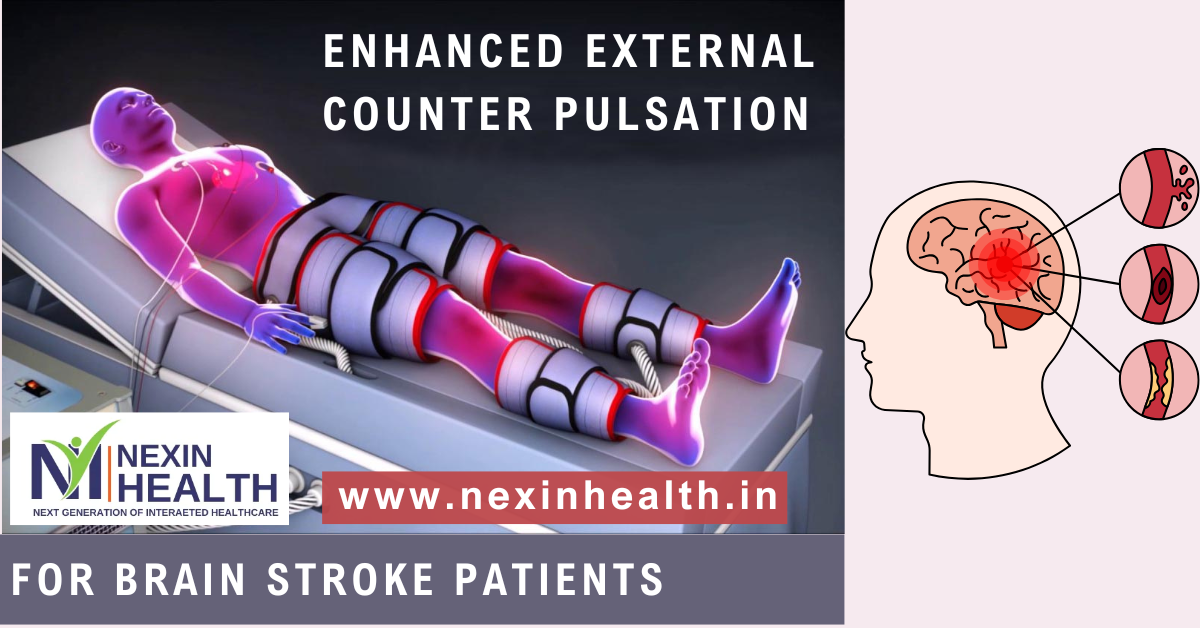
Enhanced External Counterpulsation (EECP) is a non-invasive treatment that improves blood flow to the heart. It involves:
Applying pressure to the lower body
Synchronized with the heart’s rhythm
Typically requires 35 one-hour sessions
Ayurvedic approaches focus on holistic healing and may include:
Herbal supplements (e.g., Arjuna, Guggul)
Yoga and meditation practices
Dietary modifications based on individual constitution
When lifestyle changes and medications are insufficient, surgical interventions may be necessary:
Angioplasty: A minimally invasive procedure to open blocked arteries
Bypass surgery: Creating new pathways for blood flow around blocked arteries
Ongoing research is exploring new treatment options, including:
Stem cell therapy for heart regeneration
Gene therapy to promote new blood vessel growth
Targeted nanoparticle drug delivery systems
These emerging therapies show promise in improving outcomes for CAD patients. As we explore these treatment options, it’s important to consider how patients can effectively manage their condition on a daily basis.
Living with coronary artery disease requires careful management of daily activities and stress levels. Here are some strategies to help:
Practice stress-reduction techniques like meditation or deep breathing exercises
Prioritize tasks and delegate when possible to avoid overwhelming yourself
Take regular breaks throughout the day to rest and recharge
Engage in enjoyable hobbies or activities to promote relaxation
A heart-healthy diet is crucial for managing coronary artery disease. Consider the following guidelines:
| Food Group | Recommended | Avoid |
|---|---|---|
| Fats | Healthy fats (olive oil, avocado) | Saturated and trans fats |
| Proteins | Lean meats, fish, legumes | Processed meats, high-fat dairy |
| Carbohydrates | Whole grains, fruits, vegetables | Refined sugars, white flour |
Regular physical activity is essential for heart health. Consult your doctor before starting any exercise program.
Start with low-intensity activities like walking or swimming
Gradually increase duration and intensity
Aim for at least 150 minutes of moderate exercise per week
Include strength training exercises twice a week
Coping with coronary artery disease can be emotionally challenging. Seek support through:
Joining support groups for heart disease patients
Talking to a therapist or counselor
Connecting with friends and family for emotional support
Practicing mindfulness and positive thinking techniques
Consistent medical care is vital for managing coronary artery disease. Ensure to:
Schedule regular check-ups with your cardiologist
Monitor blood pressure and cholesterol levels at home
Keep track of any new symptoms or changes in your condition
Follow medication schedules as prescribed by your doctor
By implementing these strategies, you can effectively manage coronary artery disease and maintain a good quality of life. Remember, each person’s journey is unique, so work closely with your healthcare team to develop a personalized management plan.
Coronary Artery Disease is a serious condition that affects millions worldwide, but understanding its symptoms, causes, and treatment options empowers individuals to take control of their heart health. From recognizing warning signs to exploring various diagnostic methods, this knowledge is crucial for early detection and effective management. While traditional treatments exist, it’s fascinating to consider why animals rarely experience heart attacks and how we can potentially reverse blockages naturally.
Taking proactive steps towards a heart-healthy lifestyle is essential for both preventing and managing Coronary Artery Disease. By adopting proper diet, exercise, and stress management techniques, individuals can significantly improve their heart health and quality of life. Remember, your heart’s well-being is in your hands – consult with healthcare professionals and make informed decisions to protect this vital organ for years to come.
Also Read: