Heart Attack vs Heart Failure: When renowned Bollywood actor Rishi Kapoor was hospitalized in 2020, media reports initially suggested a heart attack. Later, it was revealed he was battling advanced heart failure – a completely different condition. This confusion between heart attack vs heart failure isn’t uncommon, even among medical professionals discussing cases publicly. Yet understanding these distinctions could be crucial for the millions of cardiac patients and their families who need to recognize symptoms, seek appropriate treatment, and manage long-term health effectively.
Both conditions affect the heart’s ability to function properly, but they represent entirely different medical emergencies and chronic conditions. While one strikes suddenly like lightning, the other develops gradually like a slow-moving storm, each requiring distinct approaches to treatment and management.
Fact Sheet: Surprising Revelations About Heart Conditions
Before exploring the differences, here are some startling facts that might change how you view these cardiac conditions:
- Over 64 million people worldwide live with heart failure, making it a global health crisis
- Heart failure doesn’t mean your heart stops beating – it means the heart can’t pump blood effectively
- 50% of heart failure patients are readmitted to hospitals within 30 days of discharge
- Heart attacks can be completely silent – 20% occur without any chest pain symptoms
- Women are 2-3 times more likely to experience atypical heart attack symptoms
- Heart failure patients have a 5-year survival rate similar to many cancer patients
- 90% of heart attacks are preventable through lifestyle modifications and risk factor management
- Heart failure affects 1-3% of the adult population but increases to 10% in those over 70
- Diabetes increases heart failure risk by 2-4 times in both men and women
- Early treatment can prevent 80% of premature heart attacks and strokes
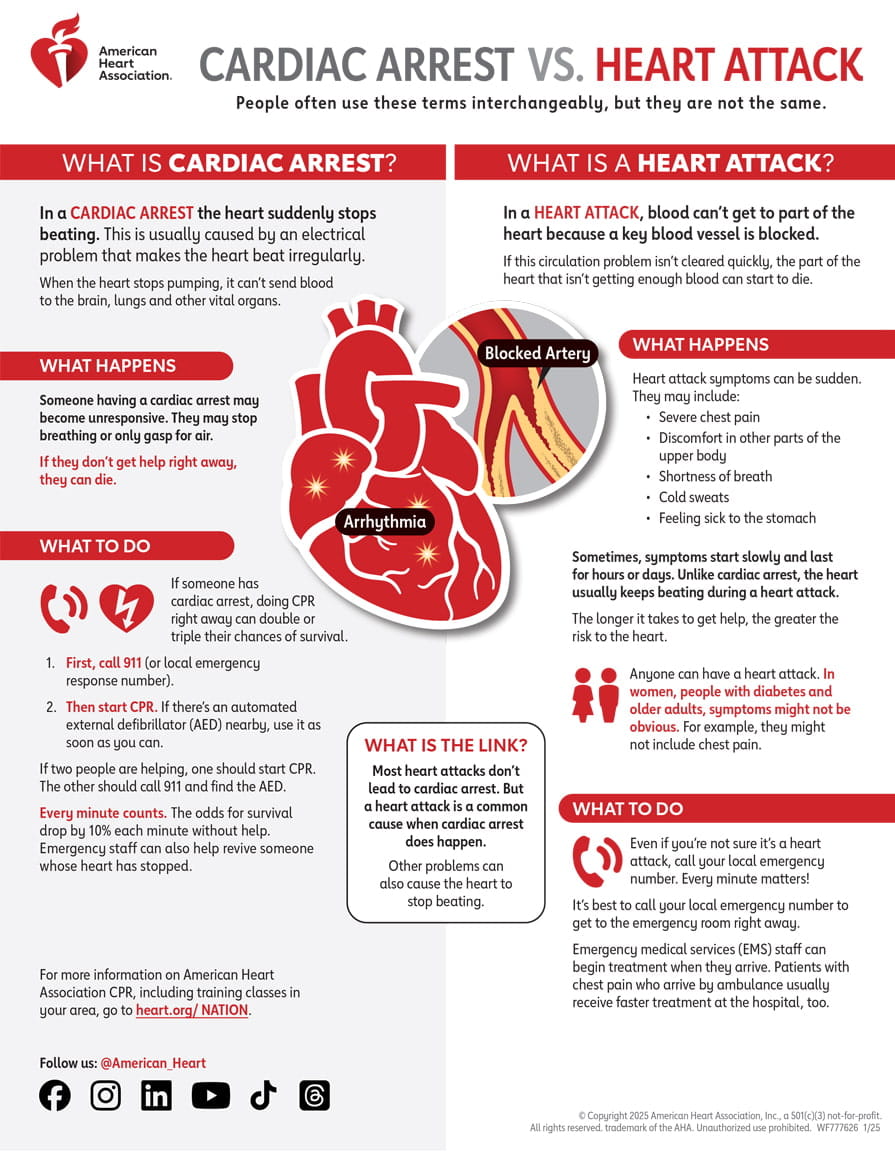
The Fundamental Distinction: Sudden Crisis vs. Gradual Decline
Understanding heart attack vs heart failure begins with recognizing their fundamental differences in timing, cause, and progression.
Heart Attack: The Emergency Strike
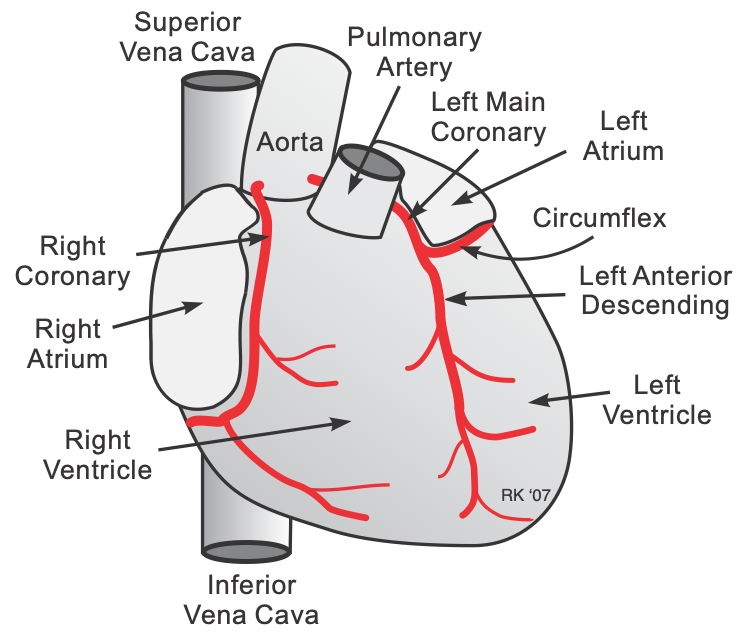
A heart attack occurs suddenly when blood flow to part of the heart becomes blocked, commonly due to a blood clot or plaque buildup in the arteries. Think of it as a traffic jam in your heart’s highway system – when a major road gets completely blocked, the area beyond that blockage suffers immediately.
Without oxygen, the heart muscles start to die, creating a medical emergency that requires immediate intervention. The affected heart muscle tissue begins deteriorating within minutes, making time absolutely critical for treatment success.
Heart Failure: The Chronic Condition
Heart failure usually develops gradually, with the heart muscle becoming weaker and having trouble pumping blood to nourish cells throughout the body. This is like having a car engine that slowly loses power over time – it still runs, but it can’t perform at full capacity.
Heart failure is a chronic condition that gradually gets worse, though medications can help patients live longer and better with it. Unlike the sudden onset of heart attacks, heart failure symptoms often develop over months or years.
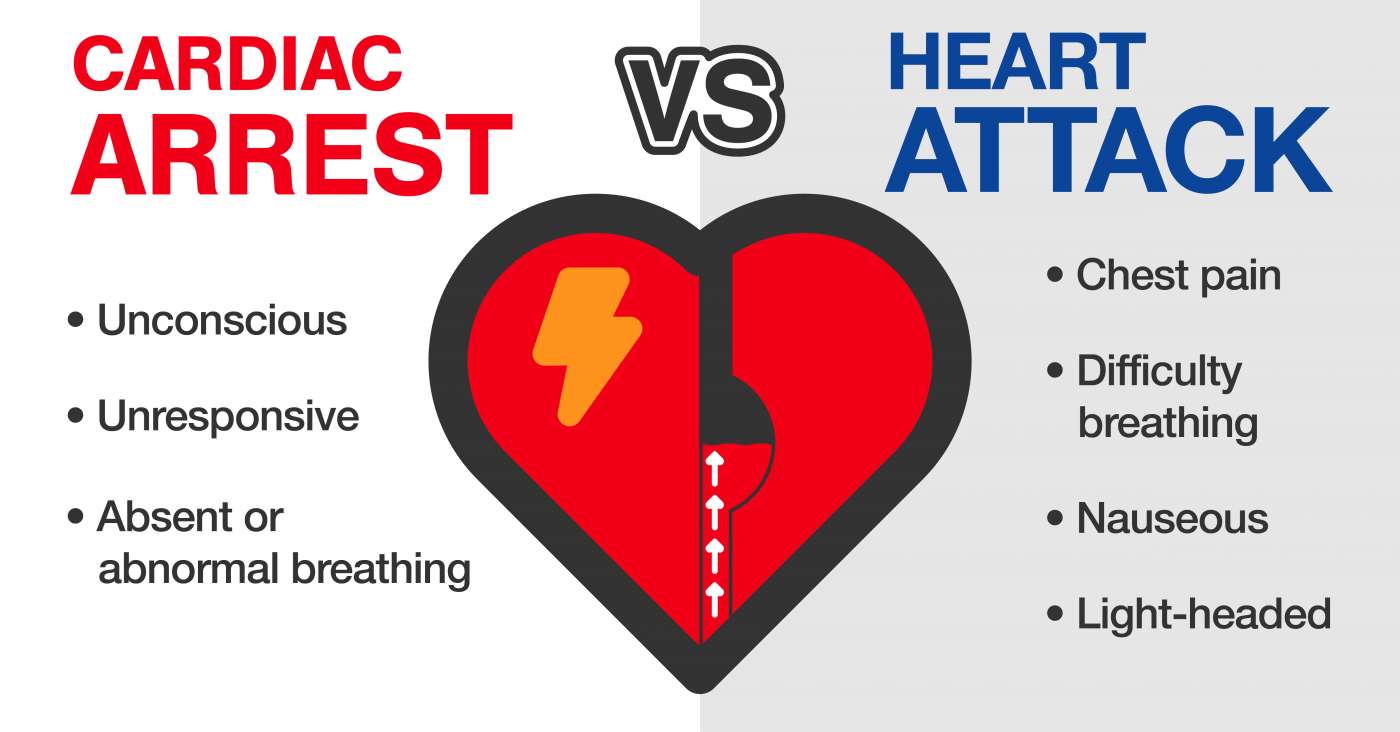
Recognizing the Symptoms: Different Warning Signals
Heart Attack Symptoms: The Body’s Alarm System
Heart attack symptoms typically appear suddenly and intensely, though they can sometimes develop gradually over hours. Key warning signs include:
Classic Heart Attack Symptoms:
- Severe chest pain or pressure that may feel like an elephant sitting on your chest
- Pain radiating to arms, neck, jaw, or back – often described as aching or burning
- Shortness of breath accompanied by chest discomfort
- Cold sweats and nausea occurring together
- Sudden dizziness or lightheadedness
Atypical Presentations: Many patients, particularly women and diabetics, experience different symptoms:
- Extreme fatigue that seems unexplained
- Indigestion-like discomfort in the upper abdomen
- Jaw or throat pain without chest symptoms
- Back pain between shoulder blades
- Sudden onset of anxiety or feeling of doom
Heart Failure Symptoms: The Gradual Decline
Most heart failure symptoms relate to fluid pooling in the body because the heart cannot pump blood forward effectively. Common symptoms include:
Primary Heart Failure Symptoms:
- Progressive shortness of breath that worsens with activity or lying flat
- Persistent fatigue and weakness that limits daily activities
- Swelling in legs, ankles, or feet (edema) that worsens throughout the day
- Rapid or irregular heartbeat during normal activities
- Persistent cough with white or pink blood-tinged phlegm
Advanced Heart Failure Signs:
- Difficulty sleeping due to breathing problems
- Decreased appetite and unexplained weight loss
- Mental confusion or difficulty concentrating
- Sudden weight gain from fluid retention
- Reduced exercise tolerance and activity levels
Understanding the Underlying Causes
What Triggers Heart Attacks?
Heart attacks result from coronary artery disease, where fatty deposits (atherosclerotic plaques) build up in coronary arteries. Risk factors include:
Lifestyle-Related Causes:
- High cholesterol levels from dietary patterns rich in saturated fats
- Uncontrolled high blood pressure damaging arterial walls
- Smoking and tobacco use accelerating plaque formation
- Diabetes mellitus affecting blood vessel health
- Obesity and sedentary lifestyle contributing to multiple risk factors
Immediate Triggers:
- Emotional stress or intense physical exertion
- Extreme weather conditions affecting blood pressure
- Severe infections causing inflammation
- Cocaine or amphetamine use causing coronary spasm
What Causes Heart Failure?
Coronary artery disease, high blood pressure, and diabetes can all cause heart failure. Heart failure usually results from another disease, most commonly coronary artery disease.
Primary Causes:
- Previous heart attacks weakening heart muscle
- Coronary artery disease reducing blood supply to heart muscle
- High blood pressure forcing the heart to work harder
- Heart valve disorders affecting blood flow efficiency
- Cardiomyopathy (enlarged or thickened heart muscle)
Secondary Causes:
- Diabetes affecting small blood vessels
- Kidney disease causing fluid retention
- Thyroid disorders affecting heart rate and rhythm
- Certain medications or chemotherapy drugs
- Alcohol abuse weakening heart muscle
Treatment Approaches: Emergency vs. Long-term Management
Heart Attack Treatment: Racing Against Time
Heart attack treatment focuses on quickly restoring blood flow to save heart muscle. Modern cardiovascular interventions include:
Emergency Medications:
- Aspirin to prevent further clot formation
- Clot-busting drugs (thrombolytics) to dissolve blockages
- Antiplatelet medications to improve blood flow
- Blood thinners to prevent new clots
Surgical Interventions:
- Angioplasty to open blocked arteries using balloon inflation
- Stent placement to keep arteries open permanently
- Coronary bypass surgery for multiple blocked vessels
- Emergency cardiac catheterization for diagnosis and treatment
Heart Failure Management: Comprehensive Care Strategy
Heart failure treatment usually involves taking medicines, reducing sodium in diet, drinking fewer liquids, and getting daily physical activity.
Medication Management:
- ACE inhibitors to reduce blood pressure and ease heart workload
- Beta-blockers to slow heart rate and reduce blood pressure
- Diuretics to remove excess fluid and reduce swelling
- Digitalis to strengthen heart contractions
Lifestyle Modifications:
- Dietary sodium restriction to reduce fluid retention
- Fluid intake monitoring to prevent overload
- Regular exercise programs tailored to individual capacity
- Weight monitoring to detect fluid retention early
Advanced Therapies:
- Cardiac resynchronization therapy for rhythm problems
- Implantable cardioverter defibrillators for arrhythmia protection
- Heart transplantation for end-stage heart failure
- Mechanical assist devices as bridge to transplant
The Connection: How Heart Attacks Lead to Heart Failure
Understanding the relationship between these conditions reveals why prevention and early treatment are crucial. Heart attacks can damage enough heart muscle to cause heart failure, while heart failure increases the risk of future heart attacks.
Acute to Chronic Progression: When a heart attack damages significant portions of heart muscle, the remaining healthy muscle must work harder to maintain circulation. Over time, this increased workload can lead to heart failure development.
Shared Risk Factors: Both conditions share common risk factors like diabetes, high blood pressure, and coronary artery disease, explaining why patients often develop both conditions.
Prevention Strategies: Building Heart-Healthy Habits
Preventing Heart Attacks Through Risk Factor Management
Dietary Modifications:
- Adopt traditional cooking methods using minimal oil and fresh ingredients
- Increase fiber intake through whole grains, legumes, and vegetables
- Limit processed foods high in sodium and trans fats
- Include omega-3 rich foods like fish, walnuts, and flaxseeds
Physical Activity:
- Engage in regular moderate exercise like brisk walking for 30 minutes daily
- Practice yoga or meditation for stress management
- Include strength training twice weekly
- Maintain active lifestyle through daily activities
Heart Failure Prevention: Protecting Your Heart’s Function
Chronic Disease Management:
- Control blood pressure through medication and lifestyle changes
- Manage diabetes with proper diet and blood sugar monitoring
- Treat sleep apnea to reduce heart strain
- Regular cardiac check-ups for early detection
Lifestyle Optimization:
- Maintain healthy weight to reduce heart workload
- Limit alcohol consumption to prevent heart muscle damage
- Avoid smoking and secondhand smoke exposure
- Manage stress effectively through relaxation techniques
Living with Heart Conditions: Quality of Life Considerations
Heart Attack Recovery: Returning to Normal Life
Heart attack survivors typically experience structured recovery phases:
Immediate Recovery (First Few Weeks):
- Cardiac rehabilitation programs to rebuild strength safely
- Medication optimization to prevent future events
- Gradual activity increase under medical supervision
- Emotional support for anxiety and depression
Long-term Lifestyle Changes:
- Dietary modifications focusing on heart-healthy foods
- Regular exercise routines tailored to individual capacity
- Stress management techniques to prevent future attacks
- Regular medical follow-ups for ongoing monitoring
Heart Failure Management: Maintaining Independence
Many people with heart failure lead normal, active lives by learning to take good care of themselves through better understanding of their condition.
Daily Management Strategies:
- Symptom monitoring to detect changes early
- Medication adherence to maintain optimal heart function
- Activity modification to conserve energy
- Support system development for ongoing care
The Role of Technology in Cardiac Care
Modern technology has revolutionized both heart attack and heart failure management:
Diagnostic Innovations:
- Portable ECG devices for continuous monitoring
- Blood biomarkers for early detection
- Advanced imaging to assess heart function
- Telemedicine platforms for remote consultation
Treatment Advances:
- Minimally invasive procedures reducing recovery time
- Drug-eluting stents preventing re-blockage
- Remote monitoring devices for heart failure patients
- Artificial heart devices for advanced cases
Building Awareness: Community Health Initiatives
Creating heart-healthy communities requires collective action:
Educational Programs:
- Public awareness campaigns about symptom recognition
- CPR training in schools and workplaces
- Health screening programs for early detection
- Community support groups for cardiac patients
Healthcare Infrastructure:
- Emergency response systems for rapid treatment
- Cardiac rehabilitation centers for recovery support
- Specialized cardiac care units in hospitals
- Trained healthcare professionals for optimal care
Frequently Asked Questions
Que: Can heart failure patients still have heart attacks?
Ans: Yes, people with heart failure remain at increased risk for heart attacks due to underlying coronary artery disease and shared risk factors. Managing both conditions requires comprehensive cardiac care and lifestyle modifications.
Que: How quickly do heart failure symptoms develop compared to heart attack symptoms?
Ans: Heart attack symptoms typically develop suddenly over minutes to hours, while heart failure symptoms usually develop gradually over weeks, months, or years as the heart’s pumping ability slowly declines.
Que: Are there any early warning signs that can help distinguish between heart attack and heart failure?
Ans: Heart attacks often cause severe, sudden chest pain with sweating and nausea, while heart failure typically causes gradual shortness of breath, fatigue, and swelling that worsens over time.
Que: Can young people develop heart failure, or is it only a condition for older adults?
Ans: While heart failure is more common in older adults, it can affect people of any age, especially those with congenital heart defects, viral infections affecting the heart, or certain genetic conditions.
Que: What is the survival rate for heart failure compared to heart attack?
Ans: Heart attack survival rates are generally higher with prompt treatment (over 90%), while heart failure has a 5-year survival rate of approximately 50%, though this varies significantly based on severity and treatment response.
Que: Can heart failure be reversed, or is it always a progressive condition?
Ans: Some types of heart failure can improve with treatment, especially if caused by treatable conditions like high blood pressure or valve problems. However, most cases require lifelong management to prevent progression.
Que: How does diabetes affect both heart attack and heart failure risk?
Ans: Diabetes increases heart attack risk by 2-4 times and heart failure risk by similar amounts due to damage to blood vessels and heart muscle, making diabetes management crucial for cardiac health.
Que: What lifestyle changes are most important for preventing both conditions?
Ans: The most important changes include maintaining healthy weight, regular physical activity, heart-healthy diet, not smoking, limiting alcohol, managing stress, and controlling blood pressure and diabetes.
Que: Can medications for heart failure prevent heart attacks, or do patients need separate treatments?
Ans: Many heart failure medications, especially ACE inhibitors and beta-blockers, also help prevent heart attacks by reducing blood pressure and protecting blood vessels, though some patients may need additional medications.
Que: How important is family history in developing either heart attacks or heart failure?
Ans: Family history significantly increases risk for both conditions, with genetic factors influencing coronary artery disease, high blood pressure, diabetes, and certain heart muscle diseases that can lead to either condition.
Understanding the critical differences between heart attack vs heart failure empowers patients and families to recognize symptoms, seek appropriate treatment
Also Read:
EECP Treatment for Heart Failure
Track Heart Failure with 6 Minute Walk Test
_____________________________________________________________________________
About the Author
Mr. Vivek Singh Sengar is the Founder of Fit My Heart and a leading Integrated Health Practitioner & Clinical Nutritionist at NEXIN HEALTH and MD City Hospital Noida. With over 13 years of experience, Vivek has treated more than 25,000 patients suffering from lifestyle diseases like heart disease, diabetes, and obesity through non-invasive, drugless, and nutrition-focused therapies.
His expertise combines modern medical knowledge with traditional Indian healing practices to provide comprehensive care for heart failure patients. Vivek’s approach focuses on sustainable lifestyle modifications, nutritional therapy, and patient education to achieve optimal cardiovascular health outcomes.
Get Expert Guidance for Your Heart Health:
📧 Email: care@nexinhealth.in
📞 Phone: +91 93101 45010
💬 WhatsApp: Click to Chat
Take the first step towards better heart health today. Contact our team for personalized heart failure management plans tailored to your specific needs and lifestyle.